Eyes with crowded anterior segments give a difficult time to the
operating surgeon due to less working field and close proximity between lens
and cornea, making capsulorhexis, phacoemulsification and IOL implantation
quite tricky to perform. These eyes present with narrow angles and shallow
anterior chambers1.
Shallow anterior
chamber can be with short axial length or with normal axial length. Short axial
length occurs in patients with microphthalmos (Simple or Complex) and nanophthalmos.
Shallow anterior chamber with normal axial length (AL) can be with relative
anterior microphthalmos, intumescent cataract, subluxated lens and in the
presence of angle closure glaucoma2.
Positive
vitreous pressure can also lead to anterior chamber shallowness during
phacoemulsification. This positive vitreous pressure is precipitated by chronic
obstructed pulmonary disease (COPD), constipation, obesity, systemic or ocular
Hypertension and senility.
Risks encountered
in such eyes during phacoemulsification include corneal endothelial damage due
to close proximity of corneal endothelium with phaco tip, Descemet’s membrane
detachment, iris prolapse, capsulorhexis extension, Posterior capsular rent,
vitreous haemorrhage and supra-choroidal haemorrhage3.
To encounter
these challenging situations and to prevent associated risks, different methods
were opted by ophthalmologists, which include pre-op use of dehydrating agents4,
intra-operative use of ophthalmic viscoelastic device (OVD)5, pars-
plana vitrectomy6,7,8 and pars-plana vitreous tap Among all of
these, pars-plana vitreous tap during phacoemulsification, in case of crowded
anterior segment when viscoelastic substance fails to maintain anterior
chamber, is found to be safe, easy and efficacious, as supported by various
studies.
The rationale of our study
was to determine the efficacy of pars-plana vitreous tap in making the anterior chamber deep thus allowing every
step of cataract surgery to be carried out safely and effectively in these high risky eyes while keeping the
advantages of a small incision.
MATERIAL AND
METHODS
A Quasi-experimental
study was conducted after approval from ethical and research committee of
Gujranwala Medical College. Informed consent was taken from all those patients.
Patients of both genders, above 40
years of age who had crowded anterior segments and in whom viscoelastic
substance could not deepen the anterior chamber sufficiently during cataract
surgery (phacoemulsification), were included in this study. Whereas patients
younger than 40 years of age, patients with posterior segment pathologies such
as vitreous haemorrhage, retinal detachment, malignant tumors and
endophthalmitis were excluded from this study. It was carried out in 50
eyes of 40 patients at eye department of DHQ-Teaching Hospital Gujranwala from
January 2014 to Dec. 2017.
Best corrected
visual acuity (BCVA) using Snellen chart,
IOP recording using Goldmann applanation tonometer, complete ophthalmic
examination using slit lamp biomicroscopy, anterior chamber angle assessment using
Gonioscopy, anterior chamber depth (ACD) estimation using ultrasound A-scan and
axial length (AL) measurement with the help of biometry was done
pre-operatively. Eyes with crowded anterior segment were selected for
pars-plana vitreous tap. The final decision to include patients in this study
was made per-operatively when anterior chamber failed to deepen with
viscoelastic substance.
Pupil was
dilated with mydriatic eye drops. Surgery was carried out under retro-bulbar
anaesthesia with 1% lignocaine and 0.5% bupivacaine followed by 10 minutes of
external ocular massage. Supero-temporal or super-nasal corneal incision was
given and anterior chamber was maintained with viscoelastic substance. Where
there was failure to deepen the anterior chamber with viscoelastic gel,
pars-plana vitreous tap was done using 27-gauge needle attached to 1 cc syringe,
inserted 4 mm from limbus in supero-temporal quadrant and 0.1 ml of vitreous was
removed. If the first attempt failed to aspirate vitreous fluid or if it was
insufficient to adequately deepen the anterior chamber in spite of successful
vitreous removal, a second vitreous tap was tried at the same site. Failure of
the technique was defined as failure of two attempts to deepen the anterior chamber.
When the anterior chamber was adequately deepened, continuous curvilinear capsulorhexis
followed by hydro-dissection, phacoemulsification via chop technique,
irrigation and aspiration of remaining cortical matter, IOL implantation in
capsular bag was successfully done in all cases without any intra-operative
complication.
Patients were followed up for 6 months to determine any post-op
complication. Data was collected from all these patients, statistical analysis
was done and results expressed as mean values with standard deviations, ranges
and percentages. P-value < 0.05 was considered significant.
RESULTS
50 eyes of 40 patients were included in this study. Out of which, 16 (40%)
were male and 24 (60%) were female. Right eye was involved in 30 cases (60%)
and left one in 20 cases (40%). Average age was 54.3 ± 7.4 (range 48 – 65) years
(table 1).
Mean
pre-op IOP was 17.6 ± 2.3 (range 12 – 24.2) mm Hg with mean pre-op anterior
chamber depth (ACD) of 2.1 ± 0.34 (range 1.6 – 2.6) mm and mean pre-op axial
length (AL) of 20.6 ± 0.45 (range 19.5 – 22.2) mm (table 2).
Table 1: Demographic variables.
|
Demographic Variables |
Study
Population (n
= 50) |
|
Age: Mean ± SD |
54.3 ± 7.4 (range 48–65) |
|
Gender: Male/Female |
40% (16)/60% (24) |
|
Laterality: Right/Left |
60% (30)/40% (20) |
Table 2: Results.
|
Variables |
Findings (n = 50) |
|
Pre-op IOP Mean ± SD |
17.6 ± 2.3 (range 12 – 24.2) mmHg |
|
Pre-op ACD Mean ± SD |
2.1 ± 0.34 (range 1.6 – 2.6) mm |
|
Pre-op AL Mean ± SD |
20.6 ± 0.45 (range 19.5 – 22.2) mm |
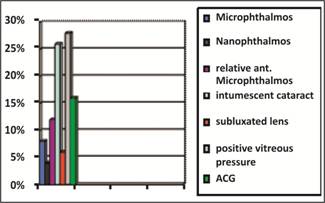
Figure 1: Types of patients.
There were 8 cases (16%) with angle closure glaucoma, 13 cases (26%) with
intumescent cataract resulting in phacomorphic glaucoma, 3 cases (6%) of
subluxated lens, 4 cases (8%) with simple microphthalmos, 2 cases (4%) with nanophthalmos,
6 cases (12%) with relative anterior microphthalmos and 14 cases (28%) with
positive vitreous pressure (that was determined per-operatively when anterior
chamber failed to deepen with viscoelastic substance) (Figure 1).
Vitreous tap was successful in 42 eyes (84%)
on first attempt and in remaining eight eyes (16%), second attempt was required
which made anterior chamber deep enough to allow phaco process to continue
safely. Average volume of aspirated vitreous was 0.116 ± 0.03 (0.1 – 0.2) ml. The
overall success rate was 100% with no intra-operative or post-operative
complications during 6 months follow up period (Figure 2, 3).
Figure 2: Success rate of vitreous tap.
DISCUSSION
Crowded anterior segment is a
descriptive term, not a measureable entity. It is used to describe eyes with
shallow anterior chambers due to short axial lengths, with intumescent cataract
causing shallow chambers with normal axial length, narrow AC angle eyes or
positive vitreous pressure where one would say, “I had difficulty in doing phaco
in this patient because he had crowded anterior chamber”.
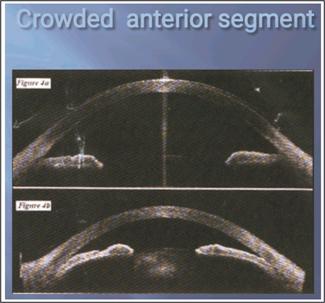
Fig. 3: a. Normal
anterior segment, b. Crowded anterior segment.
Crowded anterior segment can be seen in many ophthalmic diseases. Microphthalmos10,11 is an
eye with a short axial length. Microphthalmic eyes are divided into simple and
complex ones. Simple microphthalmos has short axial length with no other ocular
malformation. Complex Microphthalmos is an eye with a short AL and ocular
anatomic malformations such as iris coloboma, chorioretinal coloboma,
persistent fetal vasculature, and retinal dysplasia with normal scleral
thickness.
Nanophthalmos12,13,14
is a rare condition in which the eye has a short axial length along with a
small anterior segment and thickened choroid and sclera.
Relative
anterior microphthalmos is an eye with a normal AL but a small anterior
segment. These eyes have an axial length longer than 20.5 mm, but the anterior
chamber depth (ACD) is equal to or less than 2.2 mm and the corneal diameter
being shorter than 11.0 mm. It is more common than microphthalmos and
nanophthalmos15,16.
Phacomorphic glaucoma is
the secondary angle-closure glaucoma due to intumescent cataract resulting in
increased lens thickness, which can lead to pupillary block and angle closure17.
Positive
vitreous pressure also occurs during cataract surgery and is associated with acute hypotony that causes forward
displacement of the lens-iris diaphragm with shallowing of the anterior chamber
resistant to reformation, repeated iris prolapse, that can lead to a cascade of
intraoperative complications18.
Extreme care is required in all these patients. Proper preoperative
evaluation allows better planning of the surgery to avoid complications. To
reduce positive vitreous pressure, I/V infusion of mannitol 30-60 min prior to
surgery was also recommended, but its use is limited due to its serious side
effects. Pars plana vitrectomy also remained a choice for many surgeons to
deepen the anterior chamber but it has some disadvantages. The fashioned
sclerotomy may leak or require suturing. That is why using the small 23 or 25
gauge19 vitrectomy probe is preferred than using the conventional 20-gauge vitrectomy probe for this purpose, in
addition to the advantage of higher cutting rates resulting in minimal retinal
traction, but unfortunately most of the phacoemulsification systems incorporate
low-cutting speed 20-gauge vitreous cutters20.
The idea of using vitreous needle aspiration to manage positive vitreous
pressure during surgery was investigated previously in penetrating keratoplasty
(PKP) 21 and in triple procedure involving PKP, cataract extraction,
and intraocular lens implantation22. The main fear of vitreous needle
aspiration is inducing retinal traction with subsequent retinal tears, vitreous
haemorrhage, or retinal detachment16. However, this technique was
found to be safe without any complications. Earlier it was suggested that using
a 23- to 26-gauge needle attached to an insulin syringe without the plunger
allow passive removal of vitreous and avoids vitreous aspiration which may
induce traction on the retina.
Ashraf et al23
carried out a retrospective study including 26 eyes of 17 patients who
underwent phacoemulsification in which vitreous tap was done using 27 gauge
needle attached to 5 ml syringe in crowded eyes where viscoelastic substance
failed to deepen the anterior chamber and results showed no complication
related to vitreous tap, successful removal of vitreous with subsequent
deepening of anterior chamber on first attempt in 26 eyes (100%).
In this study, we used 27-gauge needle,
attached to 1 cc syringe and aspiration of 0.1 cc vitreous was done 4 mm from
supero-temporal quadrant during cataract surgery in crowded anterior segment
eyes that adequately deepened the anterior chamber. Thus, preventing damage to
corneal endothelium, Descemet’s membrane detachment, iris prolapse,
capsulorhexis extension, Posterior capsular rent, vitreous haemorrhage and
supra-choroidal haemorrhage without increasing the risk of retinal traction as
aspirated fluid was minimal. Vitreous tap using needle aspiration is machine
independent. It uses simple needles and syringes which are easily available in
operation theatres. It is quite easy to perform, cost-effective and saves time
without creating an extra wound while allowing a precise amount of vitreous to
be removed for safe accomplishment of phacoemulsification in crowded anterior
segment eyes.
CONCLUSION
A pars-plana vitreous tap makes the anterior chamber deep thus allowing
every step of cataract surgery (capsulorhexis,
phacoemulsification and IOL implantation) to be carried out safely and
effectively in these high risky eyes without causing any corneal
decompensation, capsulorhexis extension, PC rupture or supra-choroidal haemorrhage
while keeping the advantages of a small incision.
Vitreous tap using 27-gauge needle is
simple, safe, efficient and cost-effective technique for management of shallow
anterior chambers.
Author’s Affiliation
Dr. Irfan Qayyum Malik
Associate professor ophthalmology
Gujranwala Medical College
Dr. Hafiza Sadia Imtiaz
PGR
Gujranwala Medical College
Dr. Fazeela Shehzad
Associate professor Gynecology
Gujranwala Medical College
Role of Authors
Dr. Irfan Qayyum Malik
Study design, Manuscript writing, critical review.
Dr. Hafiza Sadia Imtiaz
Helped in data collection
Dr. Fazeela Shehzad
Helped in writing manuscript
REFERENCES
1.
Chang D. Pars plana vitreous tap for
phacoemulsification in the crowded eye. J
Cataract Refract Surg, 2001; 27 (12): 1911-1914.
2.
Hoffman R, Vasavada A, Allen Q, Snyder
M, Devgan U, Braga-Mele R. Cataract surgery in the small eye. J Cataract Refract Surg, 2015; 41 (11): 2565-2575.
3.
Masket S. Cataract surgical problem. J Cataract
Refract Surg, 2006; 32 (6): 908.
4.
See J. Phacoemulsification in angle closure
glaucoma. J Curr Glaucoma Pract, 2009; 3 (1): 28–35.
5.
Khng C, Osher R.H. Surgical options in the face of
positive pressure. J Cataract Refract Surg, 2006; 32 (9): 1423–1425.
6.
Chalam K.V, Gupta S.K, Agarwal S, Shah
V.A. Sutureless limited vitrectomy for positive vitreous pressure in
cataract surgery. Ophthalmic Surg Lasers and Imaging Retina, 2005; 36 (6): 518–522.
7.
Dada T, Kumar S, Gadia R, Aggarwal A,
Gupta V, Sihota R. Sutureless single-port transconjunctival pars plana limited
vitrectomy combined with phacoemulsification for management of phacomorphic
glaucoma. J Cataract Refract Surg, 2007;
33 (6): 951-954.
8.
Miura S, Ieki Y, Ogino K, Tanaka Y. Primary phacoemulsification and
aspiration combined with 25-gauge single-port vitrectomy for management of
acute angle closure. Eur J Ophthalmol, 2008; 18 (3): 450–452.
9.
Wladis E.J, Gewirt M.B, Guo S. Cataract surgery in the small adult
eye. Survey of Ophthalmology, 2006; 51 (2): 153–161.
10.
Carifi G, Safa F, Aiello F, Baumann C,
Maurino V. Cataract surgery in small adult eyes. Br J Ophthalmol 2014; 98 (9):
1261–1265.
11.
Tailor R, Ng A, Murthy S. Cataract Surgery in Patients with
Nanophthalmos. Ophthalmology, 2014; 121 (2): e11.
12.
Day A, MacLaren R, Bunce C, Stevens J,
Foster P. Outcomes of phacoemulsification and intraocular lens implantation
in microphthalmos and nanophthalmos. J Cataract Refract Surg, 2013; 39 (1): 87-96.
13.
Lemos J, Rodrigues P, Resende R,
Menezes C, Gonçalves R, Coelho P. Cataract surgery in patients with nanophthalmos: results
and complications. Eur J Ophthalmol, 2015; 26 (2): 103-106.
14.
Steijns D, Bijlsma W, Van der Lelij A. Cataract Surgery in Patients with
Nanophthalmos. Ophthalmology, 2013; 120 (2): 266-270.
15.
Yuzbasioglu E, Artunay O, Agachan A, Bilen
H. Phacoemulsification
in patients with nanophthalmos. Can J Ophthalmol, 2009; 44 (5): 534-539.
16.
B. Kaplowitz K. An Evidence-Based Approach to
Phacomorphic Glaucoma. JCEO, 2013; 04 (02).
17.
Chronopoulos A, Thumann G, Schutz J. Positive vitreous pressure:
Pathophysiology, complications, prevention, and management. Surv Ophthalmol,
2017; 62 (2): 127-133.
18.
Leng T, Moshfeghi D. Valved 25-Gauge Cannula for Vitreous
Tap and Injection. Ophthalmic Surg, Lasers and Imaging Retina, 2017; 48 (11): 916-917.
19.
Spirn M. Comparison of 25, 23 and 20-gauge
vitrectomy. Curr Opin Ophthalmol, 2009; 20 (3): 195-199.
20.
Gross R, Shaw E. Management of Increased Vitreous
Pressure during Penetrating Keratoplasty Using Pars Plana anterior Vitreous
Aspiration. Cornea, 2002; 21 (4): 435-436.
21.
Vongthongsri A, Jakpaiwong W, Preechanon
A, Lekhanont K, Chuck R. Anterior Vitreous Tapping to Manage Positive Vitreous
Pressure during Triple Procedures. Ophthalmology, 2005; 112 (5): 875-878.
22.
Sethi H, Dada T. Pars plana vitreous tap in crowded
eyes. J Cataract Refract Surg, 2002; 28 (11): 1897.
23.
Nossair A, Ewais W, Ali L. Retrospective Study of Vitreous Tap
Technique Using Needle Aspiration for Management of Shallow Anterior Chamber
during Phacoemulsification. J Ophthalmol,
2017; 2017: 1-6.